
We’ve all heard of post-traumatic stress and its disorder, PTSD. It’s like when we’re triggered by benign sights, sounds, smells, and touches due to a past event that was terrifying to experience or witness, and it gives us symptoms that last well beyond the occurrence of the event.
I learned something that can happen in us that we may not recognize, which is about post-traumatic growth. It’s when something positive comes out of our negative experiences that change the way we look at life, at what we do with our lives. It doesn’t mean we don’t suffer as a result of the traumatic event; we can even develop PTSD from it. But somewhere during and maybe after suffering, you might find a new viewpoint in life, a new purpose that’s healthy and makes you flourish. Somewhere, there’s a positive consequence of trauma.
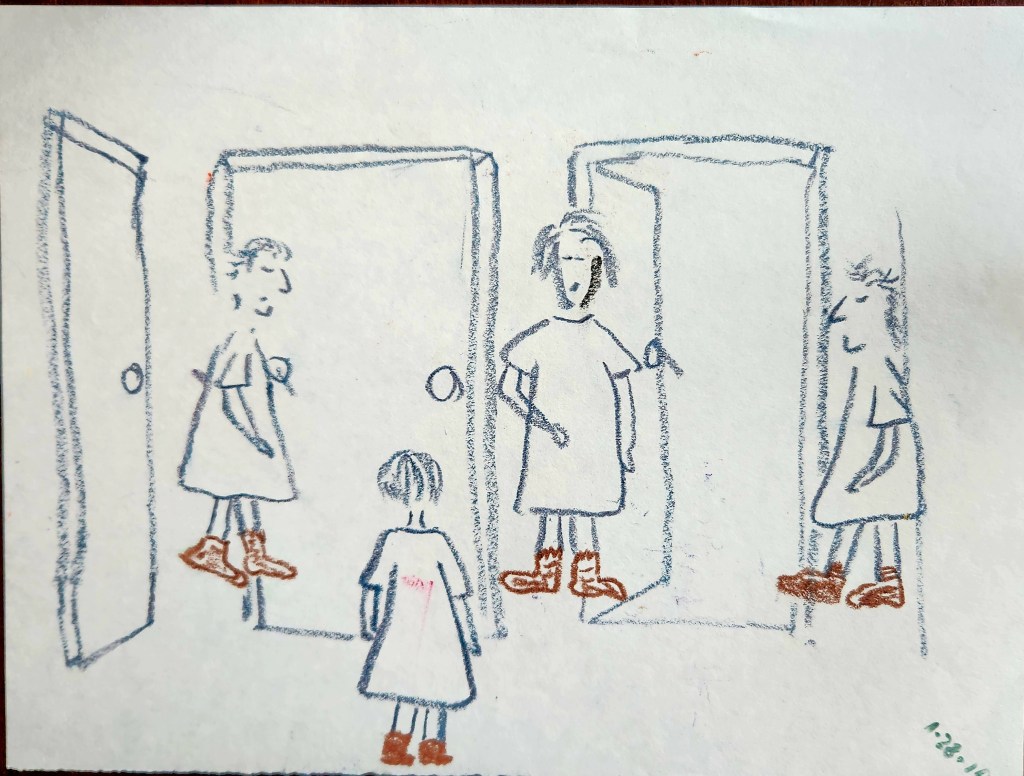
I hope to get there one day. I hope I can be able to drive back to the hospital where I went through 1 year of electroconvulsive therapy without wincing at the thought of the streets you take to get there. I had collected bags of board games, books, adult coloring books to donate to the psych ward for the inpatients. Well, I failed because I couldn’t bring myself to drive back to the hospital and I ended up donating everything to Goodwill.
How do I turn my suffering into growth? So far, I’m doing something I never felt comfortable doing – sharing my experience with mental illness: I’m doing it through this blog and I’m participating in NAMI Support Groups. My hope is to reach the individuals going through anxiety and depression who won’t necessarily talk about it with a friend or with a group of people going through the same thing. Like me once, people suffer in silence for any possible category of reasons. There are also people like me who wish to remain anonymous, and maybe eventually, I won’t feel so inhibited doing so.
Post-traumatic growth may not happen at all and it doesn’t mean you didn’t try hard enough and it doesn’t mean failure. If anything, your trauma and suffering can perhaps give you HOPE that, at the right moment, finds you meaning.






Thank you for your comment!