
2010
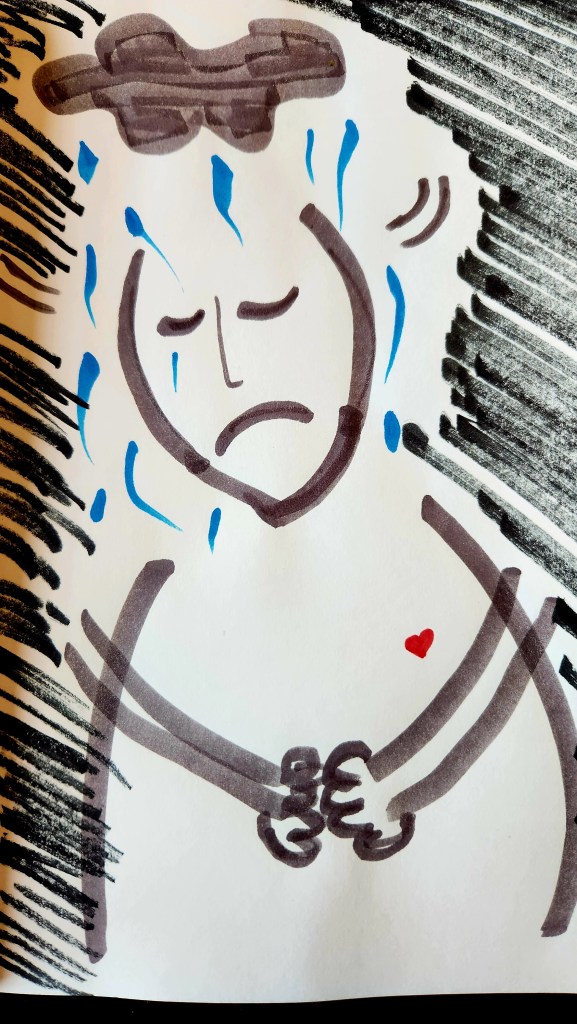
I woke up early morning feeling strange, unfazed by what was going on around me. I was alone in the studio; my husband had already left for work. The alarm was going off telling me it was my turn to go to work, but it meant nothing to me. I didn’t answer the phone calls from my employer wondering where I was. I ignored the calls from my husband checking in with me during the day. I didn’t even react when my husband came home that evening to find me where he left me. It was hard to respond to him and impossible to explain. I hadn’t eaten or taken my pills. I lay motionless all day barely processing anything.
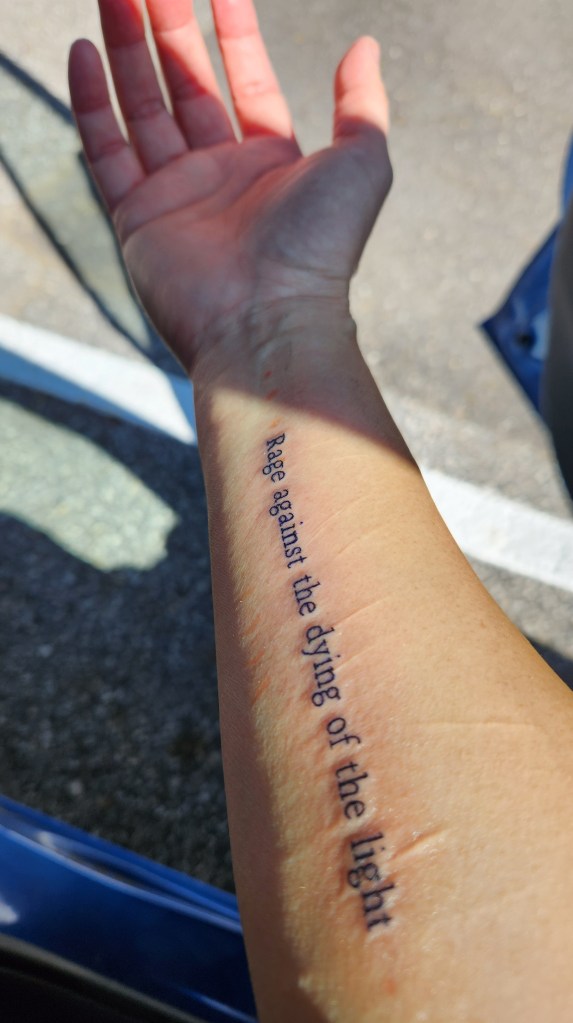
That evening, we knew a decision had to be made. I had been cutting myself to deal with the emotional pain I was going through at the time. It was a culmination of traumatic family circumstances beyond my control. It didn’t help that I was living across the country in Washington, DC, and making countless flights to and from my hometown in Portland, Oregon to deal with what was going on.
My husband was scared for me and, in the back of my mind, we knew once you’ve been admitted into a psychiatric ward, there’s no going back. It’s in your medical records. Mental health providers will have access to them. You don’t know the future repercussions it may bring . . . background checks for employment, disability and life insurance.
Ultimately, I was functionless, and I was helped to get dressed, get in the car, and my husband drove in the dark to the ER. There, my husband was given a lot of forms to complete, and I was laying on a bed curtained off from my husband and from other patients. It was all a blur. I was asked a lot of questions. I remember they asked if I wanted to kill myself. I said “no,” but I was better off dead. They put a form in front of me asking if I wanted to voluntarily be admitted into the psychiatric unit of the hospital. I signed.
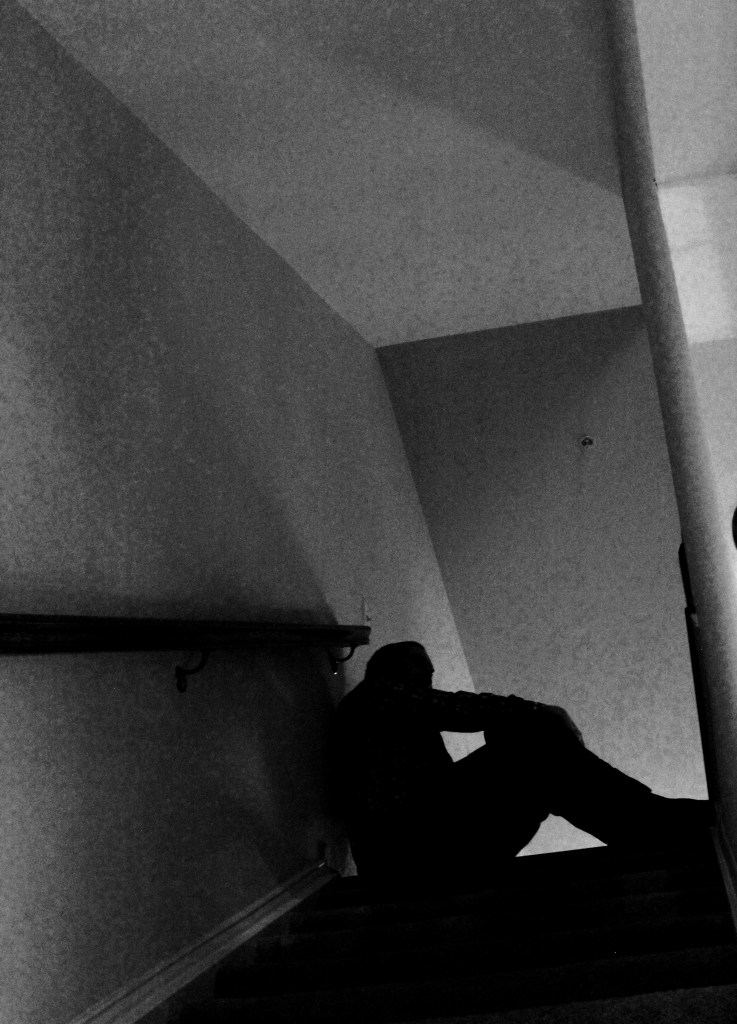
I was escorted to the psychiatric ward at the hospital. It was dark and I walked down several hallways where I was assigned a bare room with a bed and table. I had no belongings. They gave me a blue fabric gown – the ones that tie in the back, disposable underwear, and disposable socks. I changed. I slept.




Thank you for your comment!